Quibron-T, a brand name for theophylline, has been used for decades to treat asthma and chronic obstructive pulmonary disease (COPD). But it’s not the only option anymore. Today, patients and doctors have more choices - and many are safer, easier to use, and more effective. If you’re on Quibron-T or considering it, you deserve to know what else is out there - and whether switching might make your breathing easier without the side effects.
What Quibron-T (Theophylline) Actually Does
Theophylline is a bronchodilator. It relaxes the muscles around your airways, helping you breathe better. It also has mild anti-inflammatory effects in the lungs. It’s taken as a pill, usually once or twice a day. But here’s the catch: it doesn’t work the same for everyone. Your body’s ability to break it down depends on your age, liver function, whether you smoke, and even what you eat. That means the dose needs constant tweaking. A level that works one month might be too low or too high the next.
Because of this, people on theophylline often need regular blood tests. Doctors check your serum theophylline levels to make sure you’re in the safe zone - between 10 and 20 mcg/mL. Below 10, it’s not working well. Above 20, you risk serious side effects: nausea, rapid heartbeat, seizures, even heart rhythm problems. That’s why many doctors now avoid it unless absolutely necessary.
Why theophylline is falling out of favor
In the 1990s, theophylline was a go-to for severe asthma. Today, it’s rarely first-line. Why? Because better options came along. Inhaled corticosteroids (ICS), long-acting beta-agonists (LABAs), and combination inhalers like Advair or Symbicort work faster, have fewer systemic side effects, and don’t need blood monitoring.
A 2023 review in the European Respiratory Journal found that patients on inhaled therapies had 40% fewer asthma exacerbations compared to those on theophylline alone. They also missed fewer workdays and needed fewer emergency visits. Theophylline’s narrow therapeutic window and interaction risks - with caffeine, antibiotics like ciprofloxacin, or even charcoal-broiled meat - make it a high-maintenance drug in an era that values simplicity.
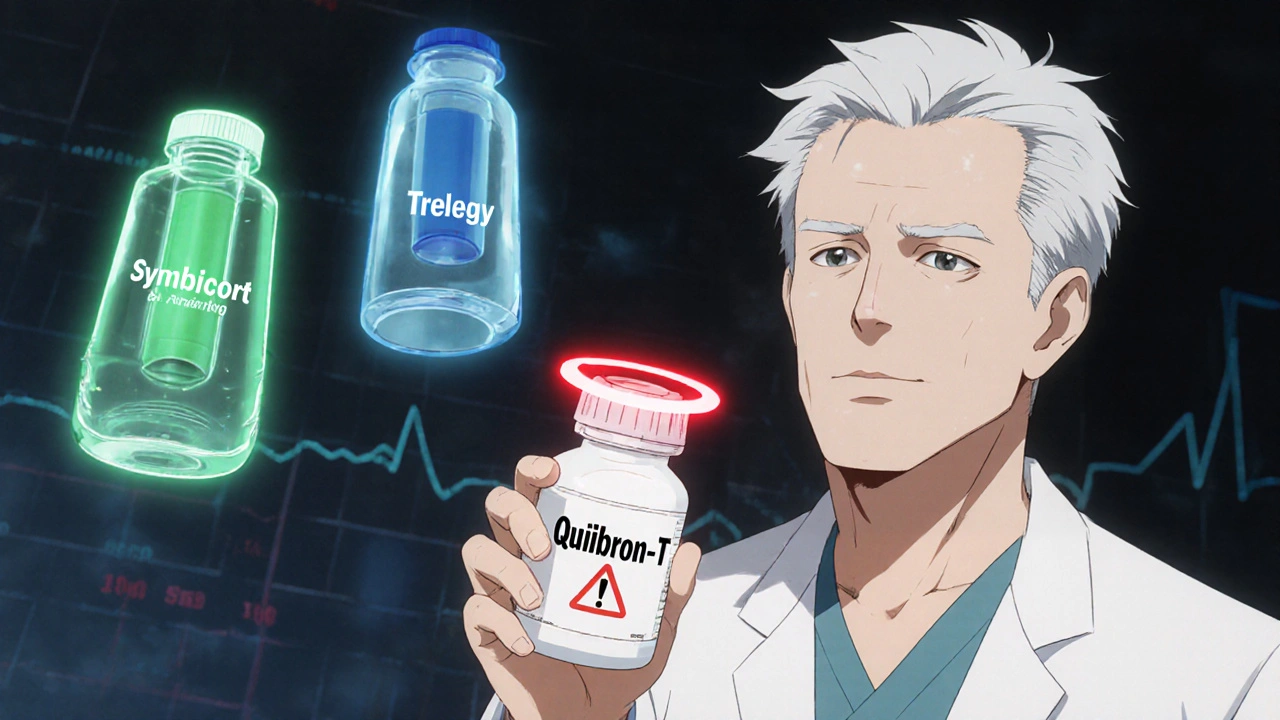
Top alternatives to Quibron-T
If you’re looking to switch from Quibron-T, here are the most common and effective alternatives - grouped by how they work.
1. Inhaled Corticosteroids (ICS)
These are anti-inflammatory drugs that target the lungs directly. Examples: fluticasone (Flovent), budesonide (Pulmicort), mometasone (Asmanex). They reduce swelling and mucus in your airways. No blood tests. No caffeine restrictions. Side effects? Usually just a sore throat or hoarse voice - easily managed with a spacer and rinsing your mouth.
ICS alone aren’t enough for daily symptom control in moderate to severe cases. That’s why they’re often paired with LABAs.
2. Long-Acting Beta-Agonists (LABAs)
LABAs like salmeterol (Serevent) and formoterol (Foradil) open airways for up to 12 hours. They’re never used alone for asthma due to safety concerns. But when combined with ICS - like in Advair (fluticasone/salmeterol) or Symbicort (budesonide/formoterol) - they’re one of the most effective daily treatments for persistent asthma and COPD.
Patients switching from theophylline to Symbicort often report feeling less shaky, sleeping better, and not needing rescue inhalers as often.
3. Leukotriene Modifiers
Montelukast (Singulair) blocks chemicals called leukotrienes that cause airway tightening. It’s taken as a daily pill, usually at night. It’s not as strong as inhaled steroids, but it’s much safer than theophylline. It’s often used for mild asthma, especially if allergies trigger symptoms.
One downside: some people report mood changes or sleep issues. But for many, it’s a good middle ground - oral, no blood tests, and effective for allergy-related wheezing.
4. Long-Acting Muscarinic Antagonists (LAMAs)
For COPD patients, LAMAs like tiotropium (Spiriva) and umeclidinium (Incruse) are often preferred over theophylline. They relax airway muscles by blocking a different pathway than beta-agonists. They’re inhaled, once-daily, and have minimal side effects. Studies show they reduce COPD flare-ups better than theophylline.
5. Combination Inhalers (ICS/LABA/LAMA)
For advanced COPD, triple therapy like Trelegy Ellipta (fluticasone/umeclidinium/vilanterol) is now standard. It combines three drugs in one device. No pills. No blood work. Just one puff a day. This is where many patients end up after trying theophylline and finding it too risky or ineffective.

Comparison table: Quibron-T vs. top alternatives
| Medication | Form | Dosing Frequency | Requires Blood Tests? | Common Side Effects | Best For |
|---|---|---|---|---|---|
| Quibron-T (Theophylline) An oral bronchodilator with narrow therapeutic window and high interaction risk | Oral tablet | 1-2 times daily | Yes | Nausea, tremors, rapid heartbeat, insomnia, seizures at high levels | Severe cases when other options fail |
| Fluticasone (Flovent) Inhaled corticosteroid for airway inflammation | Inhaler | Once or twice daily | No | Sore throat, hoarseness (rare systemic effects) | Mild to moderate asthma, maintenance therapy |
| Symbicort (budesonide/formoterol) Combination ICS/LABA inhaler | Inhaler | Twice daily | No | Headache, throat irritation, rapid heartbeat (mild) | Moderate to severe asthma or COPD |
| Montelukast (Singulair) Oral leukotriene receptor antagonist | Oral tablet | Once daily | No | Mood changes, headache, stomach upset | Allergy-triggered asthma, children, patients avoiding inhalers |
| Tiotropium (Spiriva) LAMA for COPD, blocks muscarinic receptors | Inhaler | Once daily | No | Dry mouth, constipation, urinary retention | COPD, especially with chronic bronchitis |
| Trelegy Ellipta (fluticasone/umeclidinium/vilanterol) Triple therapy for advanced COPD | Inhaler | Once daily | No | Headache, cough, fungal mouth infection | Severe COPD with frequent flare-ups |
When you might still need Quibron-T
It’s not all bad news. There are still cases where theophylline makes sense.
Some patients with severe, uncontrolled asthma who can’t afford newer inhalers - especially in low-income areas - may stay on it because it’s cheap. A 30-day supply of generic theophylline can cost under $15 in Australia, while a brand-name inhaler like Trelegy can run over $100 without subsidy.
It’s also occasionally used at night to prevent early morning asthma attacks, since its effects last 12-24 hours. Some COPD patients with nocturnal symptoms still benefit.
But here’s the reality: if you’re on Quibron-T and still having symptoms, or if you’re getting frequent side effects, it’s time to talk to your doctor about switching. The goal isn’t just to keep you alive - it’s to help you live well.
What to ask your doctor
Don’t just accept the status quo. If you’re on theophylline, ask these questions:
- Is my current dose still in the safe range? Can we check my blood level?
- Have I had any recent asthma or COPD flare-ups? If yes, is this drug really working?
- Are there cheaper or safer alternatives covered by my insurance or PBS in Australia?
- Could I try an inhaler instead? Would it reduce my risk of side effects?
- Am I taking any other meds or supplements that could interact with theophylline - like ciprofloxacin, allopurinol, or even energy drinks?
Your doctor should be able to walk you through your options. If they push back or say, “It’s worked for years,” ask for evidence - not tradition.
Real patient stories
Marie, 68, from Port Adelaide, was on Quibron-T for 15 years. She had tremors, couldn’t sleep, and kept ending up in the ER with palpitations. Her doctor switched her to Symbicort. Within two weeks, her nighttime cough vanished. Her heart stopped racing. She says, “I finally feel like I can breathe again - without the fear that my medicine might hurt me.”
Then there’s David, 42, a truck driver with COPD. He couldn’t afford inhalers without the PBS subsidy. His doctor kept him on theophylline because it was free. But after a bad flare-up, he got help from a community health program that connected him with free inhaler samples. He’s now on tiotropium. “I still take it once a day,” he says. “But now I don’t need a blood test every month. That’s freedom.”
Final thoughts
Quibron-T isn’t evil. It saved lives before inhalers existed. But medicine has moved on. Today’s treatments are more targeted, safer, and easier to manage. If you’re still on theophylline, don’t assume it’s the best option. Ask for an update. Ask for alternatives. Your lungs - and your quality of life - deserve more than outdated solutions.
Is Quibron-T still prescribed today?
Yes, but rarely as a first choice. It’s mostly used in severe asthma or COPD cases where newer inhalers aren’t affordable or effective. Most guidelines now recommend inhaled therapies over theophylline due to better safety and fewer monitoring requirements.
What are the most dangerous side effects of theophylline?
The most serious risks occur when blood levels get too high: rapid or irregular heartbeat, seizures, vomiting, and even cardiac arrest. These are rare with proper monitoring but become much more likely if you take antibiotics like ciprofloxacin, drink large amounts of caffeine, or have liver disease.
Can I switch from Quibron-T to an inhaler safely?
Yes, but never stop theophylline suddenly. Your doctor will likely taper your dose slowly while starting the new inhaler. This prevents rebound symptoms or worsening breathing. Most patients transition safely over 1-2 weeks with close monitoring.
Are there natural alternatives to Quibron-T?
There are no proven natural replacements for theophylline in treating asthma or COPD. Supplements like magnesium or omega-3s may help reduce inflammation slightly, but they don’t open airways like bronchodilators. Relying on them instead of prescribed meds can be dangerous. Always discuss supplements with your doctor before using them.
How much does Quibron-T cost in Australia compared to alternatives?
Generic theophylline costs about $10-$15 for a 30-day supply under the PBS. Brand-name inhalers like Symbicort or Trelegy cost $7-$30 per script with PBS subsidy. Without subsidy, inhalers can be $100-$150. But the real cost of theophylline is in blood tests, ER visits, and missed work - which add up fast.
Can children use theophylline instead of inhalers?
It’s possible, but not preferred. Inhalers with spacers are the standard for children with asthma. Theophylline is harder to dose safely in kids and carries higher risks of side effects like seizures. Montelukast (Singulair) is often a better oral option for children who can’t use inhalers.

so like... theophylline is literally just ancient medicine that somehow still exists bc big pharma doesn't want to lose cash? i mean, who still takes a pill that needs blood tests like it's 1987? 😅
Really appreciate this breakdown. I’ve been on Symbicort for 3 years now after being on theophylline for a decade. The difference isn’t just clinical-it’s life-changing. No more midnight panic attacks from palpitations, no more waiting for lab results like a prisoner. I can finally sleep through the night. And yes, the inhaler costs more upfront, but when you factor in ER visits and missed work, it’s a steal. Also, no more avoiding coffee. I’m back to my 3-cup-a-day habit without fear. 🙌
bro theophylline is literally a time bomb lmao. i had my cousin on it and he got hospitalized after drinking an energy drink + taking cipro. like… how is this still a thing?? 🤡
also singulair gave him nightmares where he was being chased by a giant inhaler. not a joke. he swore it was real.
How quaint. You Americans treat asthma like a consumer product you can upgrade with a subscription. In India, we still use theophylline because we have real problems-like access to healthcare, not just the latest inhaler with a fancy brand name. The real issue isn’t the drug-it’s the medical industrial complex that makes you believe you need the newest gadget to breathe. Theophylline works. It’s been tested for decades. Your ‘modern’ inhalers? Still under patent. Coincidence? I think not.
And don’t get me started on PBS subsidies. You think you’re saving money? You’re just paying for the illusion of safety.
There’s a deeper philosophical question here: if a drug saves lives but demands constant surveillance, is it truly healing-or just delaying the inevitable? Theophylline doesn’t just treat asthma; it turns patients into data points. Blood tests, caffeine logs, drug interactions-it’s not medicine, it’s a performance. Meanwhile, inhalers offer autonomy. You don’t need a lab to breathe. That’s not just clinical progress-it’s existential liberation. We’ve moved from surveillance to sovereignty. And that’s worth more than any cost comparison.
Guys. I work in a rural clinic in Ohio. We still prescribe theophylline because half our patients don’t have insurance, and a 30-day supply costs less than a Starbucks gift card. One guy told me he’d rather take the pill and get his blood drawn once a month than risk a $500 copay for an inhaler. This isn’t about ‘outdated’-it’s about class. The ‘better’ alternatives are only better if you can afford them. And if you’re living paycheck to paycheck, the ‘safe’ option is the one you can actually get. So stop acting like everyone has access to Trelegy. They don’t. And pretending they do is just elitist nonsense.
theophylline is just another way the globalists keep us dependent on toxic pharma control systems. why do you think they made blood tests mandatory? to track you. and don't even get me started on how inhalers are laced with microchips now. i heard a nurse whisper it once. they're using your breathing data to feed into the climate change AI. you think the 'side effects' are just nausea? no. it's the government monitoring your oxygen levels. wake up.
While the pharmacokinetic profile of theophylline is indeed characterized by a narrow therapeutic index and significant interindividual variability, the comparative efficacy data presented in the referenced European Respiratory Journal study appears to conflate intent-to-treat outcomes with real-world adherence metrics. Furthermore, the cost-benefit analysis neglects the systemic implications of over-reliance on proprietary combination inhalers, which are subject to market monopolization under patent law. A more nuanced evaluation would account for regional formulary restrictions and socioeconomic stratification in pharmaceutical access.
haha classic. they say 'theophylline is outdated' but they don't tell you the real reason they banned it in the EU in '98-because the FDA and WHO colluded with big pharma to push inhalers. they even changed the WHO guidelines to make it look like theophylline was dangerous. i found the leaked memo. it says 'increase inhaler sales by 300% by 2005'. and now look. we're all addicted to plastic tubes. 🤡
Hey, I’ve been a respiratory therapist for 22 years. I’ve seen patients on theophylline who were barely hanging on-and then switched to Symbicort or Trelegy and just… lit up. One woman, 71, couldn’t walk to her mailbox. Two weeks on triple therapy? She started gardening again. The key isn’t the drug-it’s the *transition*. You can’t just flip a switch. You need to taper slowly, monitor closely, and give the lungs time to adjust. But when you do it right? It’s like swapping a rusty bicycle for a Tesla. The relief isn’t just physical-it’s emotional. You stop living in fear of your own medicine. That’s the real win.
you think theophylline is bad? wait till you hear about the 'inhalers'-they're made in China with recycled plastic from nuclear waste sites. my cousin’s doctor gave him Symbicort and his tongue turned blue for 3 days. they don't tell you that the 'active ingredients' are just glitter and lies. the real cure? breathe in turmeric steam and chant mantras. the west is too lazy to heal themselves so they pay for poison. theophylline is honest-it makes you sick so you know it's working. the inhalers? they make you feel fine while slowly poisoning your soul.
The data presented is methodologically unsound. The European Respiratory Journal study cited lacks control for confounding variables including patient compliance, socioeconomic status, and baseline disease severity. Moreover, the cost analysis fails to account for the marginal utility of reduced hospitalization rates, which constitute a significant component of overall healthcare expenditure. Theophylline remains a viable option in resource-constrained environments, and its continued use is not indicative of medical backwardness, but rather pragmatic adaptation to systemic inequities. Dismissing it as 'outdated' is a form of epistemic arrogance.