Every year, hundreds of thousands of patients in U.S. hospitals suffer harm from medication errors that never should have happened. These aren’t rare mistakes-they’re preventable failures in systems that are supposed to protect people. A patient gets the wrong dose of insulin. A nurse administers a chemotherapy drug meant for weekly use, but it’s given daily. An elderly person leaves the hospital with conflicting instructions for their blood thinner. These aren’t hypotheticals. They’re real events, documented in reports, hospital logs, and patient stories. The good news? We know how to stop most of them.
What Medication Safety Really Means
Medication safety isn’t just about double-checking labels. It’s a full system of checks, tools, training, and culture designed to catch mistakes before they reach the patient. The American Society of Health-System Pharmacists defines it as preventing any event that could lead to inappropriate use or harm while the medication is under the care of a healthcare provider. That includes everything from prescribing and dispensing to administering and monitoring.The stakes are high. Back in 1999, the Institute of Medicine shocked the medical world by revealing that between 44,000 and 98,000 people die each year in U.S. hospitals from preventable errors. About 7,000 of those deaths are tied to medications. Even more alarming: studies show that on average, every hospital patient experiences at least one medication error per day. Most are caught before harm occurs, but not all.
The Biggest Risks: High-Alert Medications
Some drugs are simply more dangerous if used wrong. These are called high-alert medications. The Institute for Safe Medication Practices (ISMP) maintains the official list, and hospitals must identify their own based on local data. Common ones include:- Insulin
- Opioids like morphine and fentanyl
- Anticoagulants like warfarin and heparin
- Chemotherapy agents like vinca alkaloids and methotrexate
- IV oxytocin in labor and delivery
- Concentrated electrolytes like potassium chloride
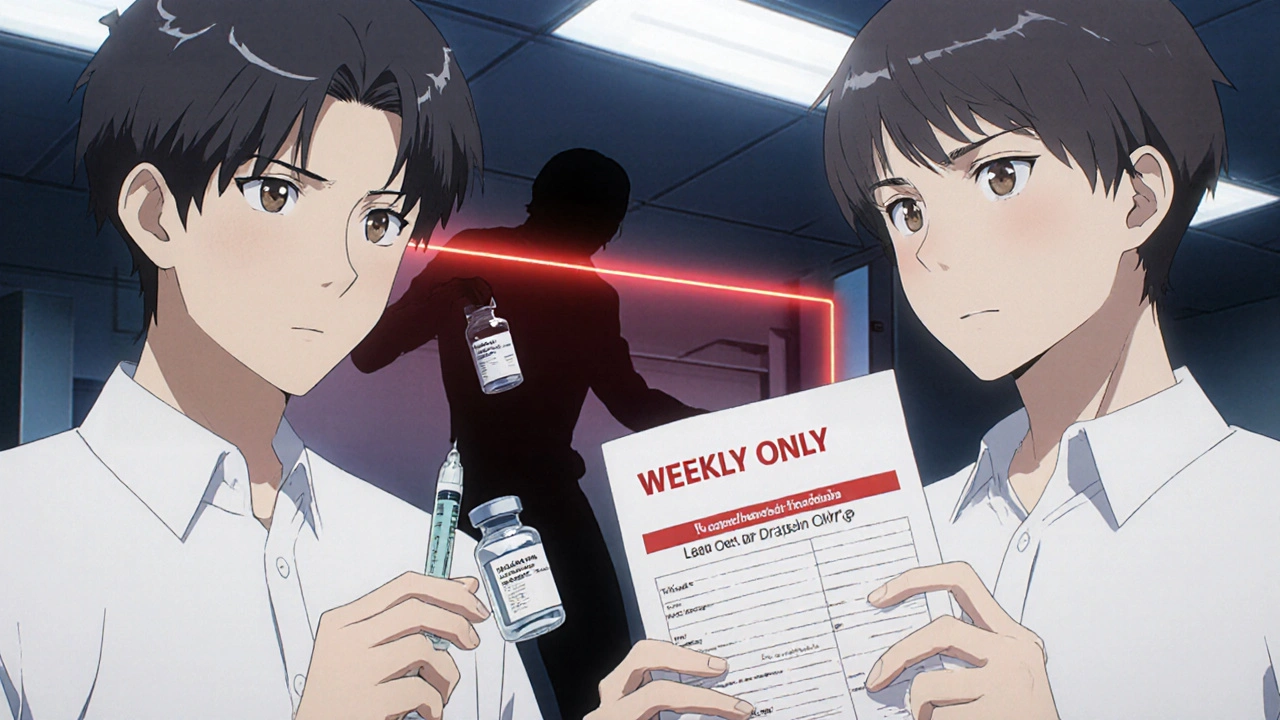
These aren’t risky because they’re powerful-they’re risky because small mistakes can cause big harm. A 10-fold dosing error with insulin can send a patient into a coma. Giving methotrexate daily instead of weekly can be fatal. That’s why safety protocols for these drugs aren’t suggestions-they’re mandatory.
ISMP’s Targeted Best Practices: The Gold Standard
The ISMP Targeted Medication Safety Best Practices for Hospitals (2020-2021 edition) is the most specific, actionable guide in the field. It’s not a vague policy document-it’s a list of 19 concrete actions hospitals must take. Here’s what they require:- Methotrexate: Electronic systems must default to weekly dosing. If someone tries to order it daily, the system must block it unless the prescriber confirms it’s for cancer treatment and enters a special code. Patients must get both written and verbal instructions, and their discharge paperwork must clearly state the dosing schedule.
- Vinca alkaloids: These drugs must never be given into the spinal fluid. Hospitals must remove all vials of vinca alkaloids from spinal injection trays and store them separately with warning labels.
- Glacial acetic acid: This chemical is used in labs but looks like water. It’s been mistaken for saline and injected into patients, causing severe tissue damage. Hospitals must remove it from patient care areas entirely.
- Insulin: Must be stored in standardized concentrations. No more mixing 100-unit and 500-unit vials. Automated dose range checking must be turned on in electronic orders.
Hospitals that fully follow these rules see a 37% drop in preventable harm, according to a 2021 study in the Journal of Patient Safety. That’s not just a number-it’s lives saved.
Technology That Works
You can’t rely on memory or good intentions alone. Effective medication safety needs tech that works. The most proven tools include:- Barcode Medication Administration (BCMA): Nurses scan the patient’s wristband and the medication barcode before giving any drug. If the system says “this isn’t right,” the dose won’t be administered. Hospitals with full BCMA use report 55% fewer serious errors.
- Electronic Health Records (EHR) with Clinical Decision Support: Systems that flag drug interactions, incorrect doses, or allergies in real time. For example, if a doctor orders 50 mg of morphine for a patient already on another opioid, the system should pop up a warning.
- Automated Dispensing Cabinets: These locked cabinets only release medications after the right user logs in and selects the correct drug, dose, and patient. They reduce theft and mispicks.
But tech alone isn’t enough. A 2021 survey found that 63% of hospitals struggle to build hard stops in their EHR systems because vendors won’t customize them. That’s why many hospitals still rely on pharmacists to manually review high-risk orders until the software catches up.
Human Factors: The Silent Risk
Even with the best tech, people make mistakes. Fatigue, distractions, poor communication, and time pressure are huge contributors. A nurse rushing between patients might miss a critical warning. A doctor might write “5 mg” instead of “0.5 mg” and not catch it. A pharmacist might assume a dose is correct because it’s “what’s usually given.”That’s why independent double-checks matter-especially for high-alert drugs. Two trained staff members must independently verify the drug, dose, route, and patient before administration. No shortcuts. No “I’ve done this a hundred times.”
And communication? It’s everything. Medication reconciliation-reviewing a patient’s full list of medications when they’re admitted, transferred, or discharged-is one of the most underused safety tools. A 2022 study found that 70% of medication errors at discharge happen because the hospital didn’t properly update the patient’s list. That’s why patients should always leave with a printed, updated medication list and someone explain it to them in plain language.
What’s Changing in 2025?
Medication safety isn’t standing still. New developments are shaping the future:- AI for Real-Time Alerts: By 2025, 75% of U.S. hospitals are expected to use artificial intelligence to scan orders and patient data for hidden risks-like detecting when a patient’s kidney function drops and automatically flagging a dose that’s too high.
- Outpatient Safety: The ISMP is expanding its best practices to include clinics and pharmacies. Between 2019 and 2023, medication errors in outpatient settings rose 40%. Patients are getting prescriptions filled at retail pharmacies, managing complex regimens at home, and getting infusions in ambulatory centers-none of which have the same safety layers as hospitals.
- Patient Involvement: Pilot programs at Mayo Clinic and Johns Hopkins are asking patients to review their own medication lists before leaving. When patients spot errors, error detection improves by 32%.
- Regulatory Pressure: The FDA now requires clearer labeling on concentrated electrolytes. CMS ties hospital payments to safety performance. The Joint Commission can revoke accreditation for repeated failures.
Why Some Hospitals Still Fall Short
Not all hospitals have the same resources. Academic medical centers often have the staff and funding to implement full safety systems. But small community hospitals? They’re struggling. A 2022 ECRI Institute study found only 42% of community hospitals fully adopted all ISMP best practices, compared to 78% of large academic centers.Cost is a barrier. Implementing new tech, training staff, and redesigning workflows can cost $285,000 or more per hospital. Staff shortages make it harder to do double-checks. Electronic systems from different vendors don’t always talk to each other. And when frontline workers are burned out, safety protocols become the first thing to get skipped.
One nurse manager in a rural hospital told the American Nurses Association forum that requiring both written and verbal methotrexate instructions created workflow bottlenecks during staffing shortages. She wasn’t against safety-she was overwhelmed. That’s why solutions must be practical, not just perfect.
What Patients Can Do
You don’t have to be passive in your own safety. Here’s what you can do:- Always ask: “What is this medicine for? How often do I take it? What happens if I miss a dose?”
- Keep your own list of all medications-prescription, over-the-counter, supplements-and bring it to every appointment.
- Before leaving the hospital, ask for a printed medication list and have someone explain it to you.
- Check your wristband before any medication is given. Make sure your name and birth date match.
- If something feels wrong-like a pill looks different than usual-speak up. Don’t assume the staff knows better.
According to a National Council on Aging survey, 68% of older adults feel safer when hospitals verify identity with name, birth date, and wristband. That’s a simple step-but it works.
The Bottom Line
Medication safety isn’t about blame. It’s about building systems that protect people even when humans make mistakes. The tools exist. The data proves they work. The question isn’t whether we can do better-it’s whether we’re willing to do what it takes.Every hard stop, every barcode scan, every double-check, every patient conversation-these aren’t red tape. They’re lifelines. And in a world where one wrong dose can change everything, we can’t afford to skip them.
What is the most common cause of medication errors in hospitals?
The most common causes are poor communication, especially during handoffs between shifts or departments, and incorrect dosing of high-alert medications like insulin, opioids, and chemotherapy drugs. Human factors like fatigue and distractions play a big role, but the biggest driver is system failures-like missing electronic alerts, lack of barcode scanning, or no independent double-checks.
What are high-alert medications, and why do they need special handling?
High-alert medications are drugs that carry a higher risk of serious harm if used incorrectly-even if the error is small. Examples include insulin, opioids, anticoagulants, and chemotherapy agents. They need special handling because a simple mistake-like giving 10 times the right dose-can cause death or permanent injury. That’s why they require extra safeguards: standardized concentrations, automated dose checks, mandatory double-checks, and hard stops in electronic systems.
How effective are barcode scanning systems in preventing errors?
Barcode medication administration (BCMA) systems reduce serious medication errors by 55%, according to the Agency for Healthcare Research and Quality. These systems ensure the right patient gets the right drug, dose, route, and time by scanning both the patient’s wristband and the medication barcode. If the system detects a mismatch, it blocks administration. Hospitals without BCMA have significantly higher error rates.
What’s the difference between ISMP best practices and Joint Commission standards?
The Joint Commission sets broad national safety goals, like “perform medication reconciliation” or “identify high-alert medications.” ISMP’s Targeted Best Practices are much more specific and actionable-they tell hospitals exactly how to do it. For example, ISMP says: “Default methotrexate to weekly dosing and block daily orders unless confirmed for cancer.” The Joint Commission says: “Have a process for safe medication use.” ISMP’s approach leads to 37% fewer preventable harms, but requires more resources to implement.
Can patients really help prevent medication errors?
Yes. Patients who actively participate in their care reduce their risk. Studies show that when patients review their own medication lists, ask questions about new prescriptions, and verify their identity before receiving drugs, error detection improves by up to 32%. Simple actions-like bringing a list of all your meds to the hospital or asking, “Is this the right medicine for me?”-can stop a mistake before it happens.

Insulin errors are the worst. One decimal point and you're either in the ER or the morgue. No joke. I've seen nurses panic because the system didn't block a 10x dose. Tech helps, but humans still screw up. And no, 'I've done this a thousand times' isn't a safety protocol.
Barcode scanning should be mandatory everywhere. Not optional. Not 'if you have time.' If your hospital doesn't use it, they're gambling with lives.
Let's be real-this isn't just about tech or protocols. It's about culture. In my old hospital, pharmacists were treated like order checkers, not safety partners. We'd get 200 orders an hour and be told to 'trust the system.' The system doesn't sleep. People do. And when they do, the wrong drug gets pushed through. We need to elevate the role of the pharmacist, not just use them as a last-minute filter.
And don't get me started on how outpatient pharmacies are just as dangerous. My grandma got her chemo dose wrong because the pharmacy didn't know she was on dialysis. No one talked to each other. No one cared enough to check.
Hospitals need to stop treating safety like a compliance checkbox. It's a mindset. It's a habit. It's the difference between someone going home and someone going to heaven.
I work in a rural clinic and we don't have half the resources these big hospitals talk about. We don't have AI alerts. We don't have automated cabinets. We have one pharmacist who covers three towns and a nurse who does double duty as a med admin and charting clerk. The ISMP guidelines are great-but they're written for hospitals with budgets and staff. What about the rest of us? We need practical, low-cost solutions, not a 50-page playbook. Can we get a 'Safety Lite' version for places that are barely hanging on?
Also, patients need to be trained too. Not just told to 'ask questions.' Teach them how to read a prescription. Show them what 'weekly' looks like on a pill bottle. Make it visual. We're not all doctors here.
Who really benefits from all this 'safety tech'? Pharma companies. They profit from complex regimens and high-alert meds. The system is designed to keep you dependent on drugs, then make you pay for the mistakes they cause. Look at insulin prices-$300 a vial. Meanwhile, hospitals spend millions on barcode scanners and EHR upgrades. Why not just make the drugs cheaper and simpler? We're treating symptoms, not the rot in the system.
And don't tell me about 'double-checks.' Who's checking the checkers? The same overworked staff? The same vendors who don't want to customize software? This is all theater. The real problem is profit-driven healthcare. Safety is just the buzzword they use to look good while they keep charging.
Let's cut the fluff. Most of these 'best practices' are just bureaucratic theater. I've worked in three hospitals. None of them actually follow ISMP guidelines fully. They just slap on a sticker that says 'we comply' and move on. The real issue? Nurses are understaffed and overworked. They're not going to spend 5 extra minutes scanning a barcode when they're juggling 12 patients. The system is broken, and no amount of tech fixes a culture of burnout.
Also, 'patient involvement'? Cute. Most patients are confused, scared, or on heavy sedatives. Asking them to 'verify their meds' is like asking a toddler to fix a jet engine. It sounds good on paper. In practice? It's a liability shield for hospitals.
barcod scanin is just a crutch. if you cant remember what drug you giving then maybe u shudnt b a nurse. also why do we need 19 rules for methotrexate? just make it harder to get. lock it in a safe. done. everyone overcomplicates this. its just pills and shots. people panic too much.
also ai alerts? lol. last time i saw one it said 'this patient is allergic to water' because the doc typed 'h2o'. we dont need smarter systems. we need smarter people.
I love how this post breaks it down so clearly. I'm a nurse in a small ER and we just got our first BCMA system last year. It was a nightmare to train for, but now I actually feel safer. I used to second-guess myself every time I gave insulin. Now the system says 'no' and I don't have to argue with my gut. That's huge.
Also, I’ve had patients catch errors. One guy noticed his blood thinner was a different color and asked about it. Turned out the pharmacy sent the wrong generic. He saved himself. We need to stop treating patients like bystanders. They’re part of the team.
Small hospitals need help, not judgment. Maybe we need a national fund to help community clinics afford basic safety tools. Not everyone can afford $285K upgrades. But we can all afford to care.
Why is glacial acetic acid even in patient care areas? That’s not a medication-that’s a lab chemical. Who approved this? Who signed off? Who didn’t ask why a bottle labeled 'acetic acid' was next to saline?