SSRI Hyponatremia Risk Calculator
How This Tool Works
This calculator uses evidence-based risk factors from the article to estimate your risk of hyponatremia (low sodium) when taking SSRIs. Results show your risk level and personalized recommendations.
Every year, hundreds of thousands of older adults start taking SSRIs to manage depression or anxiety. These medications help many people feel better-but for some, they come with hidden dangers. The biggest risks? Low sodium in the blood-called hyponatremia-and the falls that often follow. These aren’t rare side effects. They’re common, serious, and often preventable.
Why SSRIs Are Risky for Older Adults
SSRIs like sertraline, fluoxetine, and escitalopram are widely prescribed because they’re generally safer than older antidepressants. But for people over 65, the body changes in ways that make these drugs more dangerous. As we age, our kidneys don’t filter blood as well. We have less total body water. Our hormones, especially antidiuretic hormone (ADH), start acting differently. All of this sets the stage for hyponatremia.SSRIs cause the body to hold onto too much water. This dilutes the sodium in your blood. Normal sodium levels are between 135 and 145 mmol/L. When they drop below 135, you have hyponatremia. In older adults, this happens in nearly 6 out of every 100 people taking SSRIs. That’s a 2.2 times higher risk than those not taking these drugs.
Fluoxetine carries the highest risk among SSRIs. Studies show it causes hyponatremia in about 6.5% of older users. Even more concerning: many people don’t feel sick at first. There’s no sharp pain or obvious sign. Instead, symptoms creep in quietly-dizziness, weakness, confusion, or trouble walking. These aren’t just ‘getting older’ symptoms. They’re warning signs of low sodium.
The Fall Connection
When sodium drops, so does balance. Dizziness and gait instability are the most common early signs. For an older adult, that’s not just uncomfortable-it’s dangerous. A stumble can turn into a broken hip, a hospital stay, or worse. While no study has directly measured how many falls are caused by SSRI-induced hyponatremia, the link is clear in clinical practice.Geriatricians see it all the time: a patient falls, gets admitted, and only then is their sodium level checked. It’s low. They’re put on fluids, the SSRI is stopped, and they improve. But by then, the damage is done. One fall increases the chance of another by 50%. And each fall raises the risk of long-term disability or death.
Who’s at Highest Risk?
Not every older adult on an SSRI will develop hyponatremia. But some are far more vulnerable:- Those with baseline sodium below 140 mmol/L
- People with low body weight (BMI under 25)
- Women, especially post-menopausal
- Anyone taking thiazide diuretics (like hydrochlorothiazide) at the same time
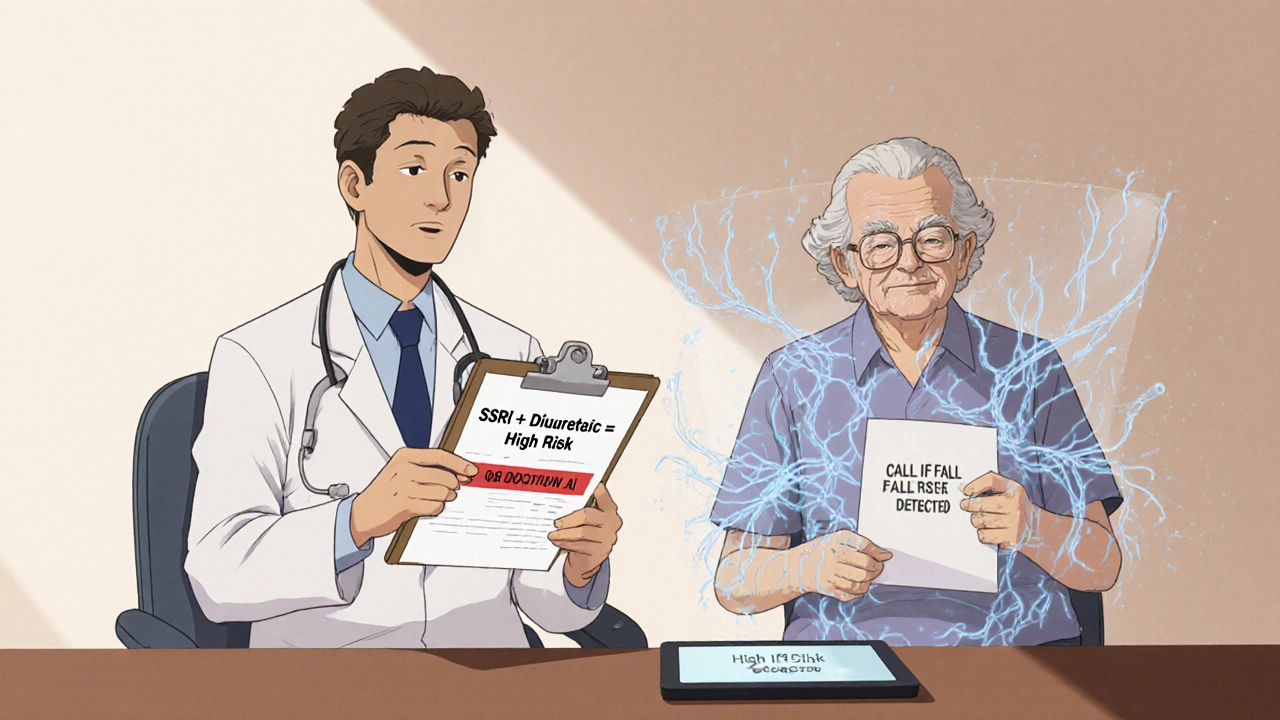
The combination of an SSRI and a thiazide diuretic is especially dangerous. Together, they increase hyponatremia risk by over 20%. That’s not a small interaction-it’s a red flag. Yet, many prescribers still pair them without checking sodium levels first.
What Should Be Done Before Starting an SSRI?
The best time to catch hyponatremia is before it starts. Here’s what works:- Get a baseline blood test for sodium before starting any SSRI.
- Repeat the test two weeks after starting-or after any dose increase.
- Review all medications. If the patient is on a thiazide diuretic, consider switching to a different blood pressure pill, like an ACE inhibitor or calcium channel blocker.
- Ask about recent falls or unexplained dizziness. These are clues, not just accidents.
Some clinics have started using electronic alerts. When a doctor prescribes an SSRI to someone over 65 who’s also on a diuretic, the system pops up a warning: “Check sodium in 14 days.” Hospitals like Johns Hopkins Bayview found that using these alerts cut emergency visits for hyponatremia by 22% in just six months.
What If Sodium Is Low?
If sodium is below 135 mmol/L, don’t panic-but don’t ignore it either.- Mild hyponatremia (125-134 mmol/L): Stop the SSRI. Limit fluids to under 1.5 liters per day. Recheck sodium in 3-5 days. Most people bounce back.
- Severe hyponatremia (below 125 mmol/L): This is a medical emergency. Hospitalization is needed. Sodium must be corrected slowly-too fast can cause brain damage.
Many doctors hesitate to stop antidepressants because they worry about relapse. But if the patient is dizzy, weak, or falling, the SSRI is doing more harm than good. In these cases, switching to a safer alternative is the right move.
Alternative Antidepressants with Lower Risk
Not all antidepressants carry the same risk. Some are much safer for older adults:- Mirtazapine: This is the safest option. It doesn’t affect ADH or sodium levels. It can even help with sleep and appetite, which many older adults struggle with.
- Bupropion: Another low-risk choice. It doesn’t cause hyponatremia. It may not help with anxiety as well as SSRIs, but it’s a solid option for depression.
- Psychotherapy: Cognitive behavioral therapy (CBT) works just as well as medication for mild to moderate depression in older adults-and has zero side effects.
The American Geriatrics Society’s 2023 Beers Criteria now lists SSRIs as potentially inappropriate for older adults with low sodium or risk factors for it. That’s not a small warning. It’s a call to change practice.
The Monitoring Paradox
Here’s the frustrating part: Studies show that checking sodium levels doesn’t always prevent hospitalizations. One 2023 study found that even when doctors followed guidelines and tested sodium, patients still ended up in the hospital. Why?Because testing alone isn’t enough. You need action. If the sodium is low, you must stop the drug or switch it. You must educate the patient and family. You must watch for falls. Many clinics test-but then do nothing. That’s why monitoring fails.
The real solution isn’t just more blood tests. It’s better systems: clear protocols, patient education, and fast follow-up. One geriatric practice in Florida started giving patients a simple handout: “If you feel dizzy, weak, or confused after starting this pill, call us immediately. Don’t wait.” They cut their fall-related ER visits by 30% in a year.

What You Can Do Right Now
If you or someone you care for is on an SSRI:- Ask the doctor: “Has my sodium been checked since I started this medicine?”
- Ask: “Is there a safer alternative, especially if I’ve had falls or feel unsteady?”
- Watch for dizziness, confusion, or trouble walking. Don’t brush it off as ‘just aging.’
- If you’re on a water pill (hydrochlorothiazide, chlorthalidone), ask if it’s still needed.
- Keep a list of all medications-including over-the-counter ones-and review it every 3 months.
Depression is real. It’s painful. But treating it shouldn’t come at the cost of safety. The goal isn’t just to feel better-it’s to live well, stay strong, and avoid preventable harm.
What’s Changing in 2025
New tools are emerging. A national initiative called the Geriatric Antidepressant Safety Collaborative is now using AI to predict who’s most at risk. It looks at sodium levels, fall history, medication lists, and even walking speed. Early results show it can flag high-risk patients with 85% accuracy.The FDA has also updated SSRI labels to include stronger warnings for older adults. Pharmacies now have to give out new patient guides that clearly state the risk of low sodium and falls.
But the biggest change? More doctors are listening. The tide is turning away from automatic SSRI prescriptions for older adults. Safer options are getting more attention. And patients are asking better questions.
Can SSRIs cause falls in older adults?
Yes. SSRIs can cause hyponatremia, which leads to dizziness, weakness, and poor balance. These symptoms significantly increase the risk of falls. Many falls in older adults on SSRIs are linked to low sodium levels-not just general frailty.
How soon after starting an SSRI does hyponatremia happen?
It usually shows up within 2 to 4 weeks of starting the medication or after a dose increase. That’s why checking sodium levels at two weeks is critical. Waiting longer can miss the window to prevent serious complications.
Is mirtazapine really safer than SSRIs for older adults?
Yes. Unlike SSRIs, mirtazapine doesn’t trigger the hormone changes that cause hyponatremia. Multiple studies and clinical guidelines, including those from the American Geriatrics Society, list it as a preferred alternative for older adults, especially those at risk for low sodium or falls.
Should I stop my SSRI if I feel dizzy?
Don’t stop it on your own. But do contact your doctor right away. Dizziness could be a sign of low sodium. Your doctor may order a blood test and decide whether to adjust your medication. Stopping suddenly can cause withdrawal symptoms, so always work with your provider.
Can I take a diuretic with an SSRI?
It’s risky. Combining thiazide diuretics like hydrochlorothiazide with SSRIs greatly increases the chance of hyponatremia. If you’re on both, ask your doctor if the diuretic is still necessary. Often, other blood pressure medications are safer for older adults.
Are there non-medication options for depression in older adults?
Yes. Cognitive behavioral therapy (CBT) is just as effective as SSRIs for mild to moderate depression in older adults. It has no physical side effects and can be done in person or over video. Many community centers and senior programs now offer free or low-cost CBT sessions.


It is utterly unacceptable that clinicians continue to prescribe SSRIs to elderly patients without mandatory baseline electrolyte panels. This is not negligence-it is institutionalized malpractice. The data is unequivocal, and yet, we allow vulnerable populations to be exposed to preventable, life-altering harm. There is no ethical justification for this pattern of care.
Where is the accountability? Where are the audits? When a 78-year-old woman falls, fractures her hip, and dies from complications-was it ‘aging’ or was it a preventable iatrogenic event? The answer is obvious. And yet, nothing changes.
I have reviewed dozens of charts where hyponatremia was documented, ignored, and then reoccurred after a dose increase. This is not a gap in knowledge-it is a failure of systems. We must mandate pre-prescription sodium testing for all patients over 65. No exceptions. No waivers. No excuses.
And if your hospital does not have an automated alert system for SSRI + thiazide combinations, you are not practicing medicine-you are gambling with lives. The American Geriatrics Society has spoken. It is time for institutions to listen.
I have seen too many families broken by this. I will not remain silent while the system continues to fail the most vulnerable among us.
Statistical risk elevation does not equate to clinical inevitability. The 6% hyponatremia rate cited is relative to a control group, not an absolute incidence. Furthermore, the correlation between SSRI use and falls is confounded by underlying depression, sedentary behavior, polypharmacy, and cognitive decline-all of which independently increase fall risk.
Studies that attribute falls primarily to hyponatremia fail to control for these variables. The assertion that ‘many falls are linked to low sodium’ is an overgeneralization. Clinical observation ≠ epidemiological proof.
Additionally, mirtazapine carries its own risks: weight gain, sedation, metabolic syndrome-all of which may exacerbate frailty in older adults. The notion that it is universally ‘safer’ ignores the trade-offs. There is no perfect drug-only context-appropriate prescribing.
And while electronic alerts are useful, they are not a substitute for clinical judgment. The real problem is not the medication-it is the reductionist approach to geriatric mental health.
Y’all need to stop treating depression like it’s a glitch to be fixed with a pill 😔
My grandma started on sertraline and went from walking her dog every morning to needing a cane in 3 weeks. We didn’t know why-until the ER doc checked her sodium and said, ‘This is why you fell.’
Switched her to mirtazapine. She’s back to gardening, laughing again, and even started knitting again 🧶❤️
Don’t ignore dizziness. Don’t wait for a fall. Ask the questions. Push for the test. You’re not being ‘difficult’-you’re being a lifesaver.
And if your doctor says ‘it’s just aging’? Find a new doctor. 💪
One must question the epistemological foundation of this article. Is it a clinical guideline? A policy brief? Or merely a well-structured opinion piece masquerading as evidence-based medicine?
It cites studies-yes-but selectively. The 2023 study showing that sodium monitoring didn’t reduce hospitalizations? Ignored. The fact that SSRIs are first-line for a reason? Omitted. The meta-analysis from the Cochrane Collaboration on fall risk stratification? Not referenced.
And yet, the tone is alarmist. The recommendations are simplistic. The conclusion? That we should abandon SSRIs in favor of mirtazapine-without acknowledging its higher risk of sedation, weight gain, and QT prolongation in the elderly.
This is not medicine. It is fearmongering dressed in clinical jargon.
And the mention of AI? A distraction. Technology cannot replace clinical reasoning. Nor should it be used to justify blanket policy changes based on incomplete data.
One wonders whether the author has ever treated a patient with treatment-resistant depression in their 80s. Or if they merely read a few papers and wrote a viral LinkedIn post.
Depression in older adults is often silent. No crying. No dramatic outbursts. Just quiet withdrawal. No appetite. No walks. No interest in grandchildren.
SSRIs are not the villain. The villain is the system that sees a 70-year-old and assumes they’re just ‘sad because they’re old.’ We treat the symptom, not the cause.
But you’re right-hyponatremia is real. And falls are devastating. We need to do better. Not by banning SSRIs. But by listening. By checking sodium. By asking about balance. By offering CBT before prescribing.
Medication is not the only tool. But it is sometimes the only tool available when therapy is inaccessible, expensive, or culturally stigmatized.
Let’s fix the system. Not just the prescription.
And yes, mirtazapine is better. But only if the patient can tolerate the drowsiness. Otherwise, we trade one problem for another.
Balance. Always balance.
From a pharmacokinetic standpoint, the age-related decline in renal clearance, reduced total body water, and altered ADH regulation create a perfect storm for SIADH-like phenomena with SSRIs. The CYP2D6 and CYP2C19 polymorphisms further modulate risk, particularly in populations with high prevalence of poor metabolizer phenotypes.
Moreover, the interaction with thiazides is not merely additive-it’s synergistic, via dual inhibition of sodium reabsorption at the distal convoluted tubule and increased water retention mediated by V2 receptor upregulation.
While mirtazapine is indeed a favorable alternative due to its noradrenergic and specific serotonergic profile (NaSSA), its antihistaminergic effects may exacerbate orthostatic hypotension-a parallel risk factor for falls.
Therefore, a holistic geriatric assessment, including gait analysis, medication reconciliation, and baseline electrolytes, remains the gold standard-not algorithmic alerts alone.
AI-driven risk prediction models are promising, but their external validity across diverse populations remains unproven. Validation in real-world cohorts is essential before widespread adoption.
My dad started on Lexapro after Mom passed. He got super dizzy, stopped eating, and fell in the shower. We didn’t know why until his primary care doc ran a blood test and said, ‘Low sodium. Probably the med.’
We switched him to mirtazapine. He’s been sleeping better, eating again, and even started going to the senior center. No more falls.
Don’t wait for a disaster. Ask your doctor: ‘Could this be making me unsteady?’ It’s not a dumb question. It’s a smart one.
And if they act like you’re being annoying? Find someone who listens. You deserve to feel better-without risking your safety.
Love you, Dad ❤️
Ah yes. The classic ‘SSRIs cause falls’ narrative. How quaint.
Let’s not forget that depression itself causes falls. Lack of motivation. Poor nutrition. Sedentary lifestyle. Sleep deprivation. All of these are *causes* of frailty.
So we blame the drug? The drug that helped someone get out of bed? That’s like blaming a crutch for the broken leg.
And mirtazapine? Sure, it doesn’t mess with sodium. But it makes you a sleepy potato. Good luck getting your 80-year-old to stand up after lunch.
Also, CBT? Great. If you live in a city with access to a therapist who takes Medicare and isn’t booked for 18 months.
Real talk: We’re treating symptoms because we don’t have a society that supports aging humans. We don’t fix loneliness. We don’t fix isolation. We don’t fix poverty.
We just give pills and call it a day.
So yes. Check sodium. But don’t pretend this is a medical problem. It’s a societal one.
And if you think a blood test is the solution? You’re missing the whole damn picture. 🤷♂️
My aunt was on zoloft and started stumbling around like she was drunk. We thought she was just getting old. Turns out her sodium was 128. Scary stuff.
We switched her to mirtazapine and she’s been like a new person! Smiling again, cooking her famous stew, even took a trip to the beach!
DO NOT IGNORE DIZZINESS. CALL YOUR DOCTOR. ASK FOR A BLOOD TEST. IT’S FREE WITH MEDICARE.
And if your doctor says ‘it’s fine’? Go to another one. You’re worth more than a risky pill.
Love you, Aunt Carol! 💕
My mother died after a fall. They found her in the hallway. Sodium was 120. SSRI was still on the chart.
They didn’t test it. They didn’t ask.
She was 76.
I don’t care about your studies.
I don’t care about your ‘trade-offs.’
She was alive. Then she wasn’t.
And no one checked her sodium.
That’s not medicine.
That’s murder by negligence.
Oh wow. So we’re just supposed to stop SSRIs because some people get dizzy? What’s next? Ban aspirin because it causes bleeding? Ban insulin because it causes hypoglycemia?
You’re treating depression like it’s a minor inconvenience. It’s not. It’s a life-destroying illness.
And you think switching to mirtazapine is the answer? It’s sedating, causes weight gain, and can lead to metabolic syndrome-then you get diabetes, then you get more falls.
Also, ‘CBT works just as well’? Tell that to the 85-year-old with severe, chronic depression who hasn’t left the house in 2 years and can’t afford therapy.
You’re not helping. You’re just making people feel guilty for taking medicine that saved their lives.
And for the record-my grandma’s sodium was low. She was also on hydrochlorothiazide. We stopped the diuretic, not the SSRI. She’s fine.
Context matters. You’re ignoring it.
Stop fearmongering.
Wait-so SSRIs are bad for older adults? But what about the 80-year-old who was suicidal and now smiles again? Are we supposed to let them suffer because of a 6% risk?
And why is mirtazapine always the ‘safe’ choice? It makes people gain 30 pounds and sleep 12 hours a day. That’s not safety-that’s sedation.
Also, CBT? Great. If you live in Manhattan. In rural Ohio? No therapists. No internet. No hope.
And who says hyponatremia is the *main* cause of falls? What about arthritis? Vision loss? Poor lighting? Loose rugs?
This article reads like a clickbait listicle disguised as medical advice.
And the AI thing? That’s just tech bros trying to sell software to hospitals.
Stop oversimplifying. Real people aren’t data points.
Also-my neighbor’s husband died after stopping his SSRI cold turkey. Withdrawal seizures. That’s not in the article.
So maybe… just maybe… we need nuance?
Just a thought.