What Really Causes Type 2 Diabetes?
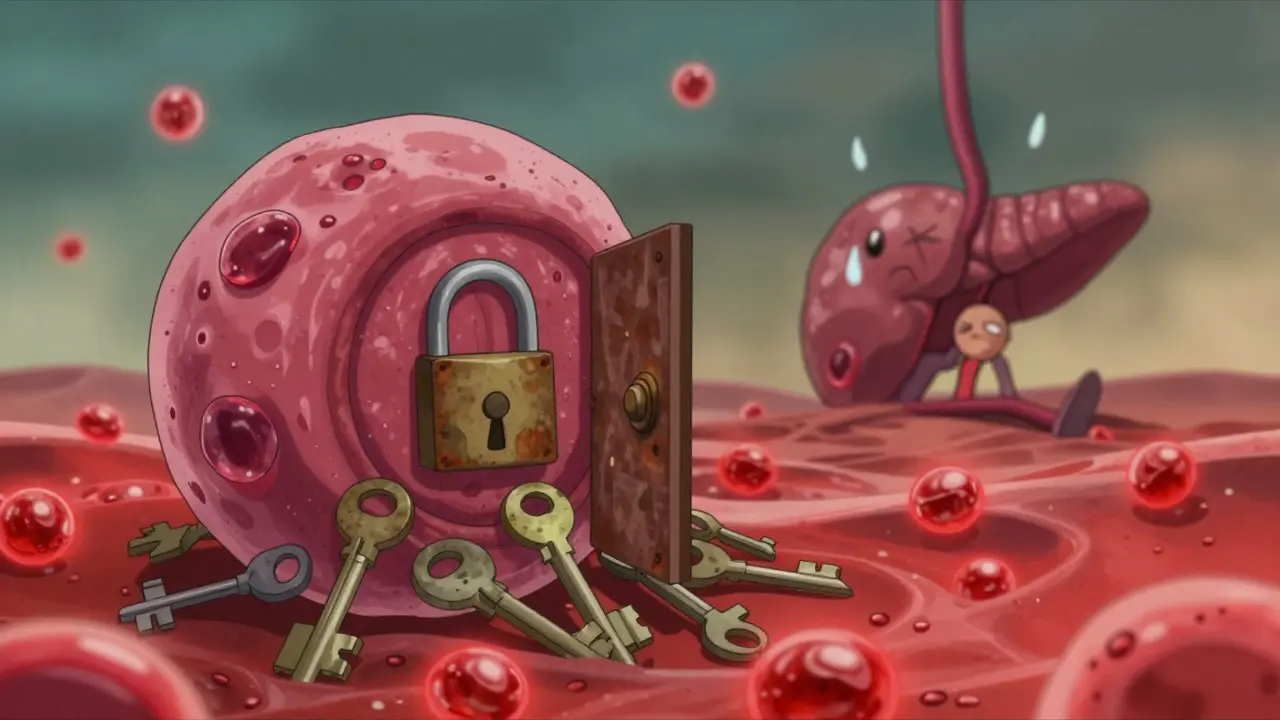
Most people think type 2 diabetes is just about high blood sugar. But the real story starts years before your glucose levels climb. It begins with something quieter, less obvious - insulin resistance. This is when your body’s cells - in muscle, fat, and liver - stop listening to insulin like they should. Insulin is the key that unlocks your cells so glucose can get in and be used for energy. When that key doesn’t fit anymore, glucose piles up in your blood. Your pancreas tries to compensate by pumping out more insulin. But over time, it gets worn out. That’s when type 2 diabetes kicks in.
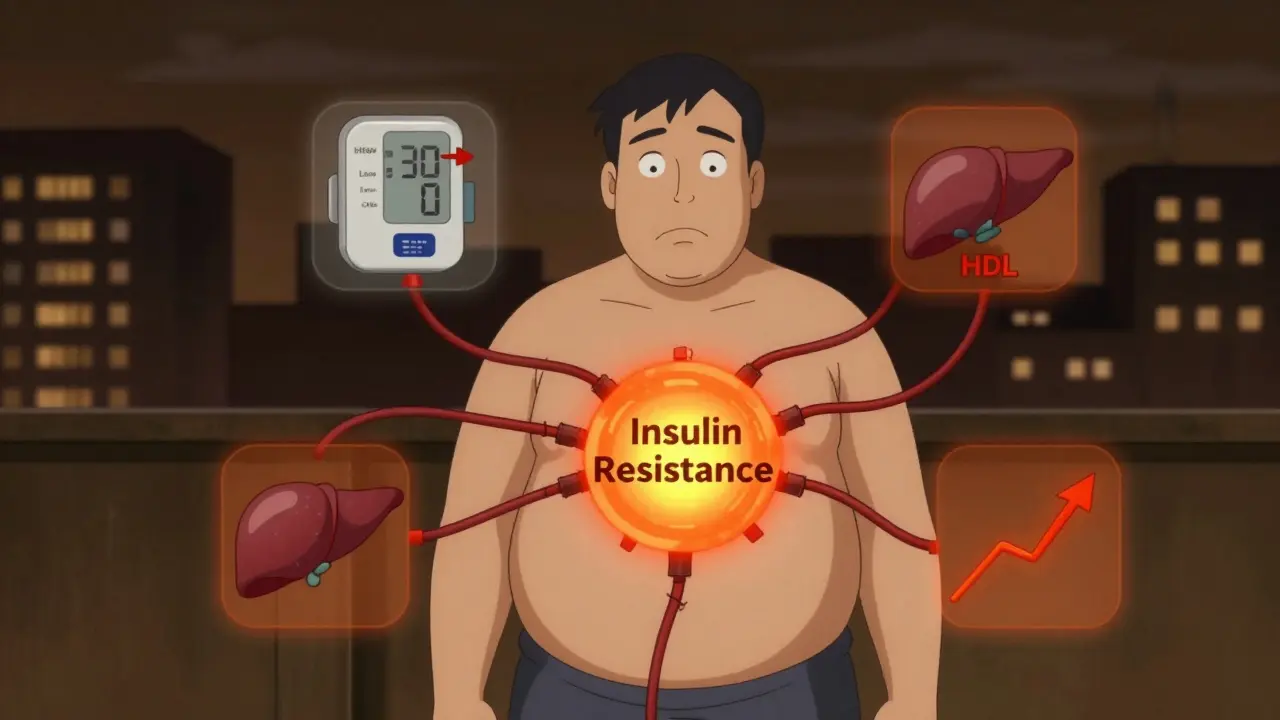
Insulin resistance isn’t just a precursor to diabetes. It’s the engine behind something bigger: metabolic syndrome. This isn’t one disease. It’s a cluster of warning signs - belly fat, high blood pressure, bad cholesterol, and rising blood sugar - that together multiply your risk for heart disease, stroke, and diabetes. The good news? You can reverse it. The bad news? Most people don’t realize they have it until it’s too late.
How Insulin Resistance Works (And Why It’s Silent)
Think of your cells as locked doors. Insulin is the key. In insulin resistance, the locks get rusty. Even when there’s plenty of key (insulin), the doors won’t open. Glucose stays in your blood. Your pancreas responds by making even more insulin. That’s called hyperinsulinemia. For years, your blood sugar might look normal. But your insulin levels? They’re skyrocketing.
This isn’t just about sugar. It’s about fat. When your body can’t use glucose properly, it starts storing more fat - especially around your organs. That’s visceral fat. It doesn’t just sit there. It spits out inflammatory chemicals that make insulin resistance worse. Fat in your liver? That’s nonalcoholic fatty liver disease (NAFLD), which affects over 80% of people with metabolic syndrome. Fat in your muscles? That blocks insulin signaling even more.
Studies show that by the time someone is diagnosed with type 2 diabetes, they’ve already lost 50-70% of their beta cell function. The pancreas didn’t fail overnight. It was fighting a losing battle for years. The real turning point isn’t when glucose hits 126 mg/dL. It’s when your body can’t keep up with insulin demand anymore.
Metabolic Syndrome: The Hidden Warning System
Metabolic syndrome isn’t a diagnosis you hear often - but it’s everywhere. About 1 in 4 adults worldwide have it. In the U.S., it’s closer to 1 in 3. The criteria are simple: you need at least three of these five things:
- Waist size over 94 cm for men (or 80 cm for women) - that’s belly fat, not just weight
- Triglycerides above 150 mg/dL
- HDL cholesterol below 40 mg/dL for men or 50 mg/dL for women
- Blood pressure at or above 130/85 mmHg
- Fasting blood sugar of 100 mg/dL or higher
Here’s what’s scary: having just one of these doesn’t raise your risk much. But three? That’s when your chance of having a heart attack or stroke jumps by 200-300%. And your risk of developing type 2 diabetes? It goes up 5 to 6 times.
And here’s something most doctors don’t say: metabolic syndrome might be better called metabolic dysfunction syndrome. The old name made it sound like a collection of random symptoms. But it’s not random. It’s one broken system. Insulin resistance is the root. Everything else - high blood pressure, low HDL, fatty liver - is a consequence.
Why Some People Get It and Others Don’t
Not everyone who’s overweight gets metabolic syndrome. And not everyone with metabolic syndrome is overweight. About 30-40% of obese people never develop it. Why? Genetics. Fat distribution matters more than total weight. Two people with the same BMI can have completely different risks.
Someone with fat stored under the skin (subcutaneous) might be fine. Someone with fat packed inside their abdomen or liver? That’s trouble. South Asians, for example, develop insulin resistance at much lower weights than Europeans. That’s why waist cutoffs are lower for Asian populations - 90 cm for men, 80 cm for women.
And lean people can have it too. Up to 20% of people with type 2 diabetes are not overweight. These are often the ones with strong genetic risks - especially those with a family history of early diabetes or heart disease. Their beta cells just can’t handle the load, even without obesity.
The Real Link Between Prediabetes and Diabetes
Prediabetes means your blood sugar is high - but not high enough for a diabetes diagnosis. Fasting glucose between 100 and 125 mg/dL. HbA1c between 5.7% and 6.4%. But here’s the key: prediabetes isn’t just a label. It’s a countdown.
The Diabetes Prevention Program showed that 70% of people with prediabetes will develop type 2 diabetes within 10 years - unless they act. But the same study proved that losing just 5-7% of body weight and getting 150 minutes of walking per week cuts that risk by 58%. That’s not a miracle. That’s biology.
People with metabolic syndrome and prediabetes who change their lifestyle don’t just avoid diabetes. They often reverse insulin resistance. Their triglycerides drop. Blood pressure improves. HDL rises. Their waist shrinks. Their liver fat decreases. Their cells start responding to insulin again.
Medication helps too. Metformin reduces diabetes risk by 31% over three years. But it doesn’t work as well as lifestyle. And it doesn’t fix the root problem - it just slows it down.
What Actually Works to Reverse It
There’s no magic pill. But there are proven steps:
- Move more: 150 minutes of brisk walking, cycling, or swimming per week. Strength training twice a week helps even more - muscle uses glucose better than fat.
- Drop the sugar: Sugary drinks are the worst. A single 20-ounce soda can spike insulin for hours. Replace them with water, tea, or sparkling water.
- Eat real food: Focus on vegetables, lean proteins, whole grains, nuts, and healthy fats. Avoid ultra-processed foods. They’re loaded with hidden sugars and fats that worsen insulin resistance.
- Lose weight - even a little: Losing 5-7% of your body weight can restore insulin sensitivity. For someone weighing 200 pounds, that’s just 10-14 pounds.
- Get enough sleep: Poor sleep raises cortisol, which increases insulin resistance. Aim for 7-8 hours a night.
And yes - weight loss isn’t easy. But you don’t need to lose 50 pounds. You just need to lose enough to make your cells responsive again. That’s often less than people think.

New Treatments Are Changing the Game
GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) and tirzepatide (Mounjaro) are turning heads. In trials, semaglutide helped people lose nearly 15% of their body weight. Tirzepatide? Up to 20%. And over 60% of people with type 2 diabetes on these drugs went into remission - meaning their blood sugar returned to normal without medication.
These drugs don’t just lower blood sugar. They reduce appetite, slow digestion, and improve insulin sensitivity. They also lower heart disease risk - something no diabetes drug has done this well before.
But they’re not a cure. And they’re expensive. Lifestyle changes still work better in the long run. These drugs are tools - not replacements for real health.
What You Can Do Today
If you’ve been told you have prediabetes, or you have high blood pressure and belly fat - don’t wait. The damage isn’t permanent. Your cells can recover. Your pancreas can rest. Your risk can drop.
Start with one change: swap soda for water. Walk for 20 minutes after dinner. Measure your waist. If it’s over 94 cm for men or 80 cm for women, it’s time to pay attention.
Ask your doctor for an HbA1c test. If it’s above 5.7%, you’re in the danger zone. Don’t wait for a diabetes diagnosis. By then, it’s harder to turn back.
This isn’t about being perfect. It’s about being consistent. Small steps, repeated daily, change your biology. Your body wants to heal. You just have to give it the right conditions.
Is insulin resistance the same as type 2 diabetes?
No. Insulin resistance is the underlying cause. Type 2 diabetes is what happens when your pancreas can’t keep up with the extra insulin your body needs. You can have insulin resistance for years without diabetes. But if it’s not addressed, diabetes almost always follows.
Can you have metabolic syndrome without being overweight?
Yes. About 20% of people with metabolic syndrome are not overweight. Genetics, fat distribution, and insulin sensitivity play bigger roles than total body weight. Someone can be lean but have high visceral fat - especially around the liver and abdomen - which drives metabolic dysfunction.
Does metformin cure insulin resistance?
No. Metformin helps lower blood sugar and improves insulin sensitivity slightly, but it doesn’t reverse the root cause. Lifestyle changes - diet, movement, and weight loss - are still the most effective way to restore how your body responds to insulin.
How long does it take to reverse insulin resistance?
Some people see improvements in insulin sensitivity within 2-4 weeks of starting a low-sugar, whole-food diet and regular walking. But lasting reversal usually takes 3-6 months of consistent effort. Weight loss, reduced liver fat, and lower insulin levels are signs it’s working.
Can metabolic syndrome lead to heart disease even without diabetes?
Absolutely. Metabolic syndrome is a stronger predictor of heart disease than high cholesterol or smoking alone. The combination of high blood pressure, bad fats, inflammation, and insulin resistance damages blood vessels over time - even if blood sugar stays normal.
Are there tests to check for insulin resistance?
There’s no single routine test. But doctors can estimate it using your fasting insulin level, triglycerides, HDL, waist size, and blood pressure. A high fasting insulin (above 10 µIU/mL) or a high triglyceride-to-HDL ratio (above 3) are strong clues. Home tests for insulin aren’t reliable - talk to your doctor if you suspect insulin resistance.
What’s Next?
If you’re reading this because you or someone you care about has been flagged for prediabetes or metabolic syndrome - don’t panic. You’re not doomed. You’re just early. The window to change things is wide open.
Start with one small step. Measure your waist. Write down what you eat for three days. Take a 15-minute walk after dinner. Talk to your doctor about an HbA1c test. Don’t wait for symptoms. By the time you feel tired, hungry all the time, or can’t lose weight - the damage is already there.
This isn’t about willpower. It’s about biology. Your body is trying to tell you something. Listen. Change the environment. Change the food. Move your body. Give it time. And don’t let anyone tell you it’s too late. It’s never too late to reset your metabolism.

Okay, let me tell you something-I was prediabetic last year, 220 pounds, waistline like a basketball, and I thought, ‘eh, I’ll just take metformin and call it a day.’ Spoiler: it didn’t work. Then I swapped soda for sparkling water, started walking after dinner, and did 20 minutes of bodyweight squats three times a week. Six months later? My HbA1c dropped from 6.1% to 5.3%. I lost 18 pounds. My doctor said, ‘You didn’t just reverse it-you reset your metabolism.’ It’s not magic. It’s just consistency. You don’t need to run marathons or go keto. Just move more, eat real food, and stop treating sugar like a best friend. Your cells are begging you to listen.
Metabolic syndrome? More like ‘Modern American Life Syndrome.’ We’ve turned our bodies into sugar-burning furnaces with a side of stress and zero sleep. The real tragedy? Doctors still treat the symptoms like they’re separate problems-‘Oh, high BP? Here’s a pill.’ ‘High triglycerides? Take this.’ ‘Oh, you’re insulin resistant? Cool, we’ll label you prediabetic and send you to a pamphlet.’ Meanwhile, the root cause-processed food culture-is still on every shelf, every billboard, every damn TV commercial. We’re not failing biology. Biology is failing us. And until we fix the system, not the symptoms, we’re just rearranging deck chairs on the Titanic.
As someone who’s studied endocrinology and lived with PCOS (which is basically insulin resistance’s cousin), I can’t stress enough how critical visceral fat is. It’s not just ‘a little extra weight’-it’s an endocrine organ that secretes IL-6, TNF-alpha, and other inflammatory cytokines that actively sabotage insulin signaling. And here’s the kicker: even if your BMI is ‘normal,’ if your waist-to-hip ratio is above 0.9 for men or 0.85 for women, you’re in the danger zone. The triglyceride-to-HDL ratio? If it’s above 3, you’ve got insulin resistance even if your fasting glucose is ‘fine.’ I’ve seen lean patients with fasting insulin levels over 25 µIU/mL. No one talks about this. But it’s the silent epidemic. You need a fasting insulin test-not just HbA1c or fasting glucose. It’s the canary in the coal mine.
Y’ALL. I just got off the phone with my endo and she said if I don’t fix this in the next 6 months, I’m looking at insulin shots by 40. I’m 34. I’m not fat. I’m 5’6”, 140 lbs. But my waist is 38 inches. My triglycerides? 210. HDL? 32. My fasting insulin? 18. I’ve been eating ‘healthy’ salads and gluten-free snacks. Turns out? Those are just sugar bombs in disguise. I just started eating eggs for breakfast, walking after dinner, and ditching the ‘low-fat’ yogurt. Two weeks in? My brain fog is gone. My energy? Skyrocketing. I’m not doing this for a bikini body-I’m doing it so I can watch my kid grow up without a pump in my belly. If you’re reading this and you’re scared? Good. Now DO SOMETHING. Not tomorrow. TODAY. Swap one thing. Right now. I dare you.
It’s funny how we blame individual choices for a systemic failure. We say, ‘Just eat less sugar!’ but sugar is engineered into 80% of packaged foods. We say, ‘Just exercise!’ but most people work 50-hour weeks and don’t have time to cook. We say, ‘Just lose weight!’ but weight loss isn’t linear, and stress makes your body hold onto fat like it’s the last lifeboat. This isn’t about willpower. It’s about environment. And until we regulate food marketing, subsidize vegetables instead of corn syrup, and make movement part of daily life-not a luxury-we’re just shaming people for surviving in a broken system. The science is clear. The policy? Still asleep.
I’m from India, and I’ve seen this play out in my family. My uncle was thin, ate rice every day, never drank soda, but had diabetes at 45. Why? Because he ate white rice with every meal, zero veggies, and sat all day. Meanwhile, my cousin is chubby but eats dal, roti, lots of greens, walks 10k steps daily, and her HbA1c is 5.2. It’s not about weight. It’s about quality. In India, we used to eat whole grains, lentils, fermented foods, and spices like turmeric and cinnamon-natural insulin sensitizers. Now we’re eating instant noodles and packaged snacks. Our grandparents didn’t have diabetes. We do. It’s not genetics. It’s cultural erosion. We need to bring back real food-not just for health, but for identity.
Stop romanticizing ‘reversal.’ You can’t ‘reverse’ insulin resistance like it’s a software update. You can manage it. You can improve it. But if you’ve had it for 10 years, your beta cells are permanently damaged. Don’t tell people they can ‘cure’ it with a walk and some kale. That’s dangerous. It makes them feel guilty when they don’t magically heal. Some people have genetic defects. Some have autoimmune triggers. Some have hormonal disorders. Not everyone can ‘fix’ this with lifestyle. And pretending they can is just victim-blaming dressed up as wellness.
I just want to say-thank you. I’ve been too scared to talk about this. I’m 31, have a 2-year-old, and my doctor told me I have metabolic syndrome last month. I cried for an hour. I thought I was failing. But reading this made me feel seen. I’m not lazy. I’m not weak. My body’s just been betrayed by food, stress, and sleepless nights. I started drinking water instead of chai with sugar. I walk with my baby in the stroller. I’m not perfect. But I’m trying. And that’s enough. You’re not alone. We’re all just trying to heal.
GLP-1 drugs? Ohhh, so now we’re just gonna medicate our way out of a cultural disaster? 🤦♂️ Let me get this straight-we’ll let Big Pharma sell us $1,000/month shots to shrink our bellies while we keep eating processed crap, sitting on our butts, and blaming our ‘metabolism.’ Meanwhile, the real solution-eating real food, moving daily, sleeping well-is free, accessible, and has zero side effects except more energy, better mood, and less brain fog. But nah. Let’s just turn people into walking Ozempic commercials. We’re not sick because we’re weak. We’re sick because we’re surrounded by poison and told it’s normal. Wake up.
Just a quick note: I’ve read a lot of this stuff, and I think the most important thing is that insulin resistance isn’t a moral failure. It’s a biological response to chronic overstimulation. Sugar, stress, sleep loss, inflammation-they all pile up. Your body isn’t broken. It’s just trying to survive. And the good news? It’s incredibly adaptable. Even small changes-like cutting out sugary coffee creamer or taking the stairs-send signals to your cells that say, ‘Hey, we’re not in famine mode anymore.’ You don’t need to overhaul your life. Just nudge it. One tiny shift. Then another. Your body remembers. And it will respond.
OMG I JUST DID THIS!! 🙌 I swapped my morning granola bar for scrambled eggs and avocado. No sugar. No carbs. Just fat and protein. And guess what? My 10 a.m. crash? Gone. My cravings? Vanished. I didn’t even try to lose weight. But I lost 7 pounds in 3 weeks. My waist is smaller. My skin is clearer. I feel like I’m 25 again. I didn’t know food could do this. I thought it was just ‘calories in, calories out.’ But it’s not. It’s about signals. Your body listens to what you feed it. Give it real fuel. It will thank you. And yes, I’m crying happy tears right now. 💕
Look, I get it. People want quick fixes. But here’s the truth: reversing insulin resistance isn’t about diet trends. It’s about rhythm. Eating at consistent times. Sleeping at consistent times. Moving consistently. Your body runs on circadian biology. When you eat at 2 a.m., sleep at 4 a.m., and skip breakfast because you’re ‘too busy’-you’re telling your cells: ‘We’re in chaos.’ They panic. They hoard fat. They ignore insulin. Fix your schedule first. Then fix your food. The rest follows. I’ve seen it in 300 patients. No magic. Just rhythm.